It is accepted by all that a brain tumor is a “disease” that warrants attention as well as acceptance. Whether one has surgery, radiation, or close surveillance until/if treatment is necessary, their life has changed when hearing the words, “You have a brain tumor.”
Just as real for Acoustic Neuroma patients is the very common outcome of Depression. It is rarely discussed as freely as the “thing” growing in one’s head. It’s common to hear:
“It could have been worse, right?” Well, that’s helpful.
“Aren’t you just happy to still be alive?” Alive, but different takes adjustment, grieving, and acceptance.
“Why can’t you just get over it?” We ask ourselves that too sometimes, just before we walk into a wall, put drops in our dry eye, or grimace when seized by head-pain.
“Post Traumatic Stress Disorder from planned brain surgery?” Yes, it is possible. If one’s life has been suddenly and dramatically changed, PTSD is possible. Life looks different when you can’t do things that used to be a no-brainer (pardon the pun).
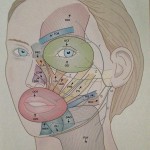
“Traumatic brain injury doesn’t result from skilled surgeons who delicately enter your skull does it?” Yes. Surgeons are skilled and they can do everything perfectly, but the brain is a delicate entity that hates intrusion.
Depression is like a blanket. Sometimes, it comfortably surrounds you and makes you want to stay under forever, curling up in isolation. Sometimes, it stifles and makes you want to squirm and push it’s itchiness away as you crave company. However it fits or feels, depression is real and a common issue following brain surgery.
Life has changed, for most, in ways that cannot be measured or even explained.
So, what do you do about it? Talk to family, friends, and professionals. Sometimes medication is necessary. As unique as each Acoustic Neuroma tumor is, each emotional outcome is similarly unique. Finding a community in your area or online brings camaraderie and smiles of understanding.
Acceptance of the “new you” is a process that does not happen overnight. Like the tide coming in and out from the ocean’s shore, waves of depression can come and go. Waves of acceptance come and go as do feelings of frustration with any limitations that may linger. Sometimes you don’t recognize the blanket of depression until it has lifted – even a bit.
Time is a great healer. Finding the patience for time to heal is not always easy for AN survivors or the people in their lives. Recognition is the first step. Not being embarrassed by something beyond your control is another step. Pulling it back into your control is the biggest step.
My ongoing advice is “inhale, exhale. . . ” and don’t hesitate to ask for help.