Single Sided Deaf or Single Sided Hearing? Let’s look at the good side of this condition many of us live with. Today, I choose the glass half full. I am fortunate enough to have great people in my life who are with me on this journey. I really appreciate each and every one of them. They have helped me laugh even as I sigh, and that has helped me seek joy even in life changes that I didn’t choose. One of those is hearing in only one ear:
- Even though I miss what someone just said on my deaf side, I may hear some good gossip from across the room on the good side (the ability to distinguish the source or distance of sounds is gone)
- I “really” see the person on my deaf side because I turn my head almost 180 degrees to hear them, positioning my baby blues to gaze directly into theirs.
- I’ve trained my family and friends to walk on the proper side, which sometimes turns into a funny dance until everyone is properly aligned. Sometimes they figure it out themselves when I don’t respond to a question and accept their responsibility to reposition. “Oh yea. . .”
- I make people feel special at dinner by sitting with them on my good side. Or people wait for me to choose where I sit first, allowing me to determine the best spot for hearing.
- I don’t have to fight the line to put my name on a restaurant waiting list because my friends and family do it while I quietly relinquish control and take a seat in the waiting zone.
- I could get a cool tattoo with an interesting graphic designed to indicate my deaf side (I haven’t chosen to do this but many have)
- When talking on the phone, the caller has my full attention. Of course, that is unfortunate for anyone on the bad side saying, unheard, “Have them pick up pizza on the way.”
- Multitasking– trying to perform tasks while listening is difficult so I tend to be very focused on one or the other. I have an excuse for not knitting.
- I’ve become accustomed to reading television using closed captioning, thereby not missing what people are saying in unfamiliar accents or low, menacing voices. I can sit back and enjoy popcorn event though crunching drowns out voices.
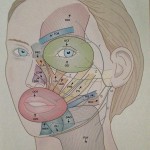
- I’ve learned that “head shadowing” is the term for what causes many things said on the side of the deaf ear to be lost completely or sound like they are coming from another room. Not to be technical but low-frequency, long-wavelength sounds bend around a person’s head and are easier to hear. High-frequency, short-wavelength sounds are not as elastic and do not bend around to the good ear. The frequencies of speech vary, causing patchiness in what is heard. I just tell people, “Let me know if I’m supposed to hear anything.” This allows me to not worry about what I might be missing. I can’t be held responsible for what I don’t hear, right? (wink)
- Oh, and the obvious. . . Sleeping is awesome when I put my good ear down on the pillow and sleep like a baby.